Welcome to the World of Children !!
We are very glad to see here all parents and those who are still planning to have a child, and we also welcome all educators and teachers.
You will find here a lot of interesting and useful information about children and for children.
We hope that you will remember our site and you will remain with us.
Interesting news is waiting for you.
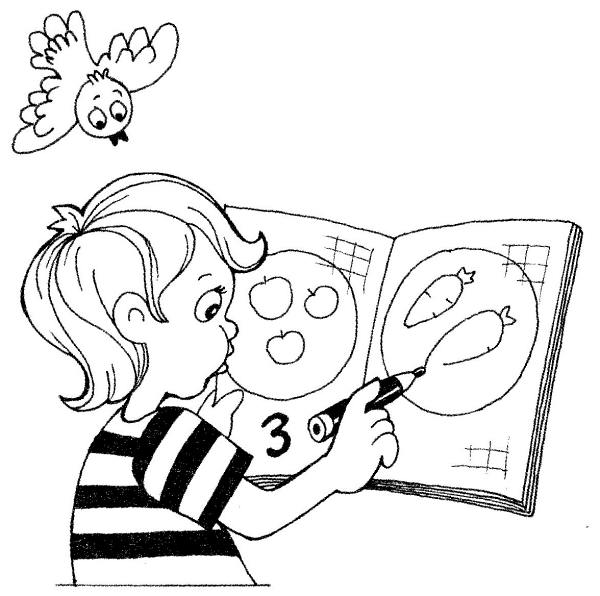
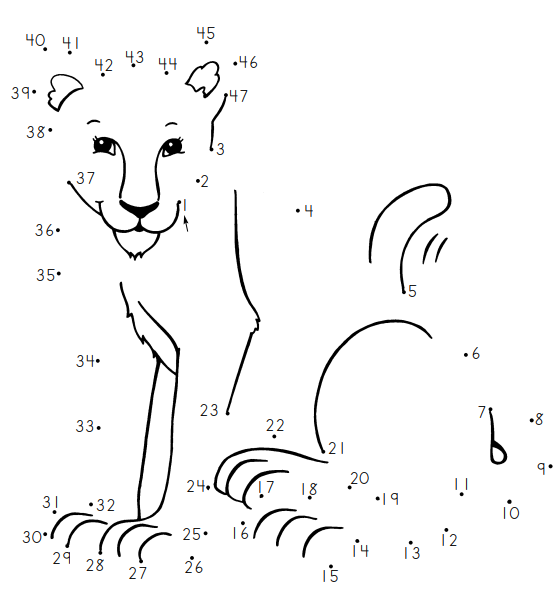
On our site you will find everything you need for the development and recreation of children.
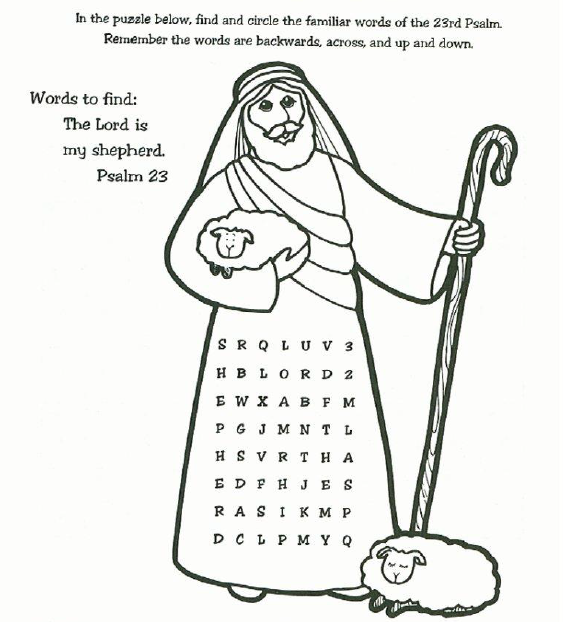
And our collection of colorings for printing will delight you with a huge number of pictures of excellent quality.
After the children play outdoor games, they can relax and watch our games.
Of course, this is not all that you will find here for children and children's recreation and learning.
We are constantly updating our site. Come to us more often!
Last Added Game Activities
Games for Kids
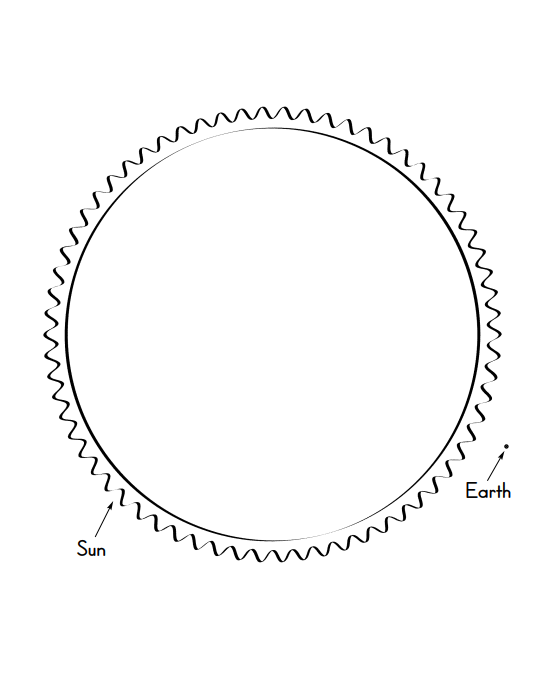
Educational games (2-6 year children)
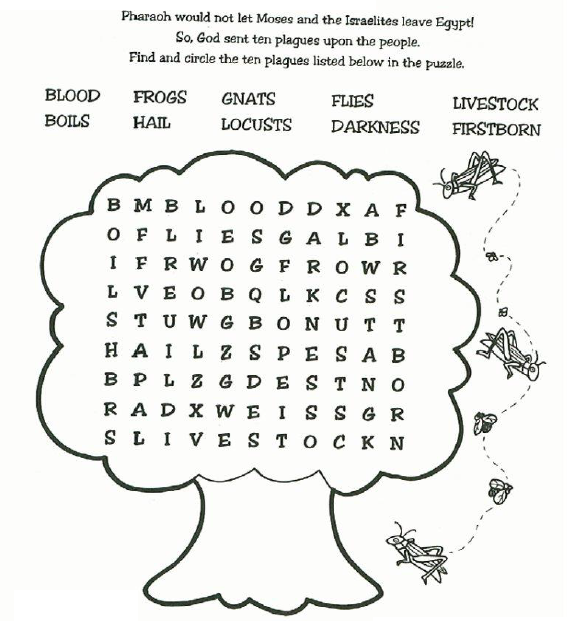
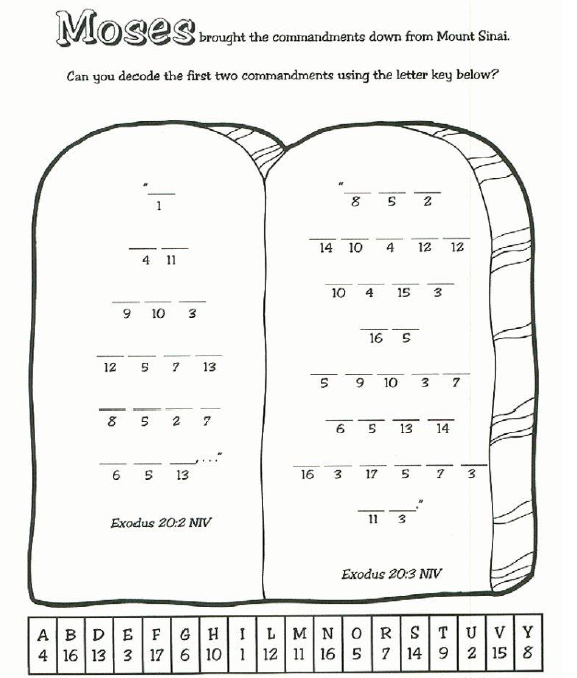
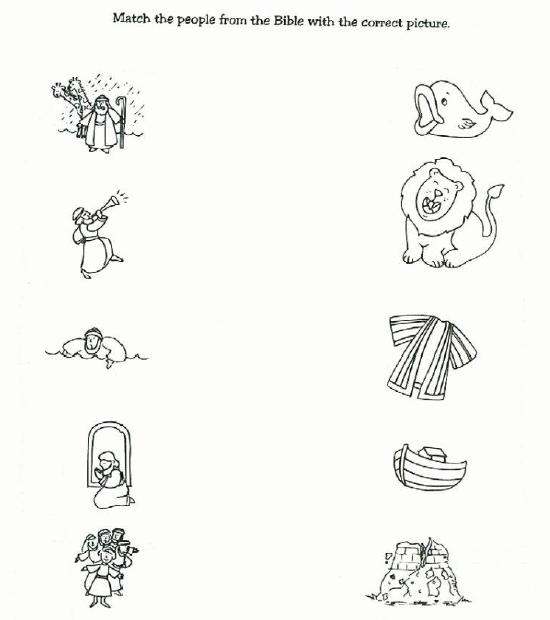
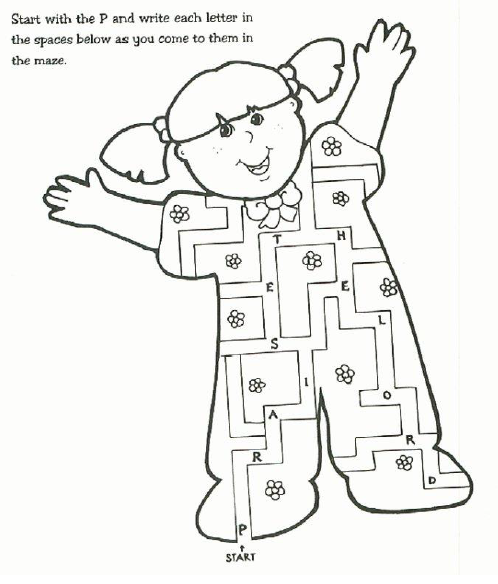
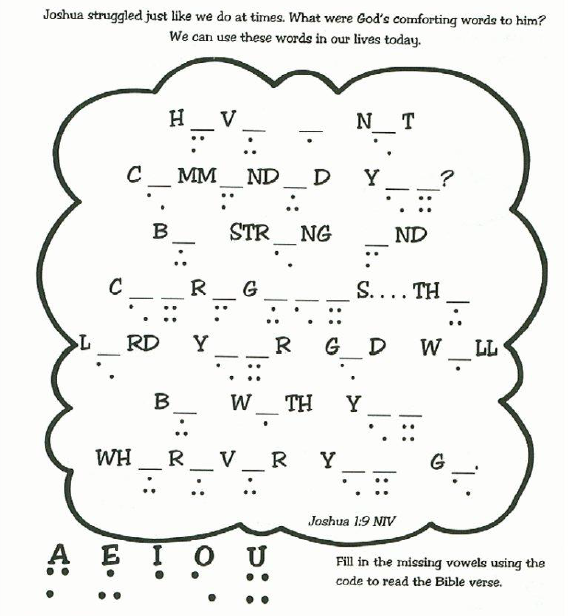
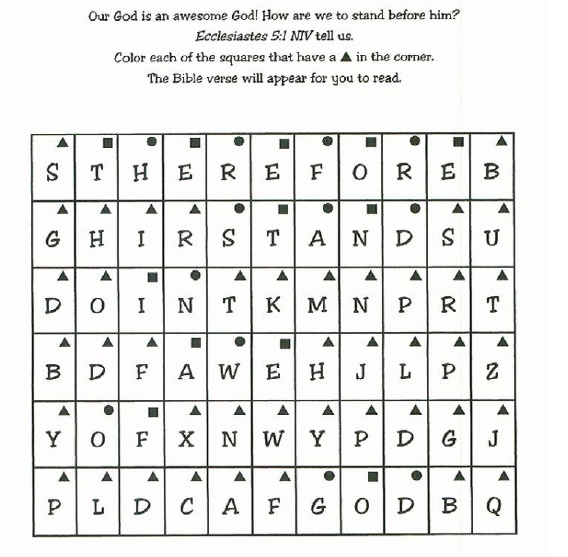
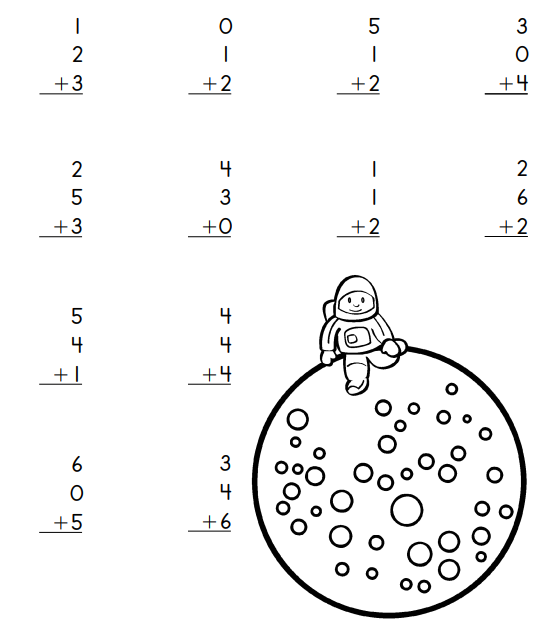
Last Added Worksheets
Popular worksheets: Halloween Worksheets, Thanksgiving Worksheets